What Are ANOC and EOC Documents, and Why Are They Important?
ANOC (Annual Notice of Change) and EOC (Evidence of Coverage) documents provide detailed explanations of healthcare plan updates—such as premiums, prescription drug coverage, or provider networks—helping patients make informed decisions about their care. Unclear or inaccessible information can lead to costly mistakes, like unexpected expenses when a prescription is no longer covered, or delays in care if a patient unknowingly visits an out-of-network provider and faces denied claims or high bills.
By providing accurate and accessible information in these documents, healthcare and insurance organizations can help patients make informed decisions, avoid complications, and feel supported in their care.
Who is Required to Provide ANOC and EOC Documents?
A variety of organizations are required to provide ANOC and EOC documents to ensure Medicare beneficiaries have access to important updates about their healthcare coverage. These include:
- Medicare Advantage Organizations (MAOs): Includes HMOs, PPOs, and Special Needs Plans (SNPs) offering Medicare Advantage plans.
- Part D Prescription Drug Plan Sponsors: Companies managing standalone prescription drug plans for Medicare beneficiaries.
- Medicare-Medicaid Plans (MMPs): Plans serving dual-eligible beneficiaries must also distribute these materials.
What Information Do These Documents Include?
- For Medicare Advantage Plans: Updates to coverage benefits, premiums, copayments, and provider networks.
- For Part D Plans: Changes to drug coverage, formularies, and cost-sharing requirements.
- For Medicare-Medicaid Plans: Information relevant to dual-eligible beneficiaries, following similar CMS guidelines.
What Languages Are Required by Center for Medicaid Services (CMS)?
CMS mandates that ANOC and EOC documents be translated into languages that meet specific thresholds so Limited English Proficiency (LEP) beneficiaries have access to critical healthcare information. The requirements are determined based on the following:
Threshold Determination:
Documents must be translated if at least 5% or 500 individuals in a plan’s service area are LEP and speak the same non-English language, according to census or enrollment data.
Note: Plans are expected to use the most up-to-date data available to assess the language needs of their members.
Commonly Required Languages:
Frequently required translations include Spanish, Chinese, Vietnamese, Korean, and Tagalog. However, the specific languages vary depending on the demographics of the service area.
Notices in Other Languages:
Even when a language does not meet the threshold, CMS requires notices in the top 15 non-English languages nationally, informing members that materials are available in their preferred language or that oral interpretation services can be provided.
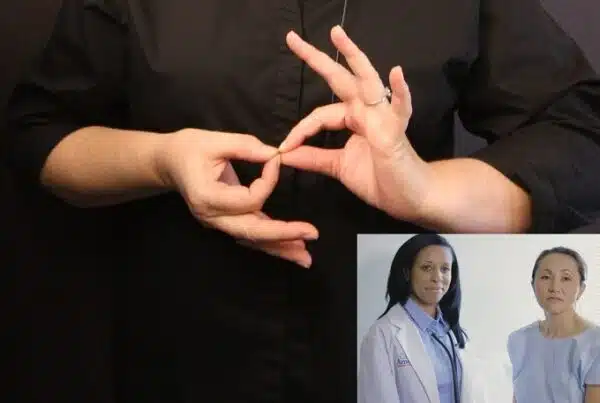
Why Accurate Translations Matter for LEP Individuals
For many LEP individuals, ANOC and EOC documents can be overwhelming, filled with complex terms that are difficult to understand. Relying on pure machine translation, which often translates word-for-word, missing key nuances in healthcare terminology or policy changes. This can leave patients unaware of key updates, such as their prescription medication no longer being covered, leading to unexpected costs or delays at the pharmacy.
Similarly, poorly translated explanations of network provider details may result in patients unknowingly scheduling appointments with out-of-network doctors, causing financial strain or denied claims. These challenges not only hinder patients’ ability to make informed decisions but also erode trust in their health plans.
By investing in accurate, culturally relevant translations, healthcare organizations can help LEP individuals fully understand their coverage, avoid unnecessary complications, and make confident decisions about their care. Clear, effective communication strengthens trust and ensures patients feel supported every step of the way.
CMS Compliance Regulations & Accessible Formats
CMS compliance extends beyond translations, requiring ANOC and EOC documents to be available in accessible formats. This allows all beneficiaries, including those with disabilities, to access and understand their plan information.
Required Accessible Formats
- Large Print: Documents must be available in large print (typically at least 18-point font) to assist individuals with visual impairments.
- Braille: Upon request, Braille versions must be provided for individuals who are blind.
- 508 Compliance: Electronic documents must meet accessibility standards outlined in Section 508 of the Rehabilitation Act. This includes proper tagging for screen readers, descriptive text for images, logical heading structures, and keyboard navigation.
Penalties for Non-Compliance
Failing to meet these requirements can result in:
- Regulatory Penalties: CMS may impose fines or sanctions on organizations that fail to comply.
- Member Dissatisfaction: Members who cannot access or understand their documents may lose trust and require additional support, increasing operational burdens.
- Legal Risks: Non-compliance with accessibility standards can lead to lawsuits and reputational damage.
How Propio Supports Your ANOC & EOC Translation Needs
Meeting CMS compliance requirements can be challenging, but Propio provides the expertise and solutions to simplify the process. Propio understands the challenges healthcare and insurance organizations face in meeting CMS requirements for ANOC and EOC documents. We provide translation and accessibility solutions that prioritize accuracy, compliance, and timeliness. Here’s how we support your needs:
- Cultural Understanding:
Our professional linguists deliver translations that are not only accurate but also culturally relevant and contextually appropriate. This ensures your members fully understand their healthcare information and feel respected in their preferred language. - Certified Security Measures:
Propio protects sensitive data through secure, HIPAA-compliant processes. Our translation management systems are certified under ISO 9001 and ISO 17100, demonstrating adherence to global quality and translation standards, while ISO 27001 and ISO 27701 certifications guarantee data security and privacy throughout the translation process. We prioritize confidentiality, making certain member information is handled with the utmost care. - Assistance with Alternate Formats:
Beyond translations, we assist with providing documents in accessible formats, such as large print, Braille, and 508-compliant digital versions, allowing all members, including those with disabilities, to access and understand the information. - Meeting Deadlines:
Our efficient workflows and dedicated teams deliver translations and alternate formats on schedule, ensuring quality without delays.
By partnering with Propio, you gain access to expert translation and accessibility solutions that help you meet CMS requirements while supporting members from all backgrounds. Together, we can ensure your members have the information they need to make confident and informed decisions about their care. Contact us today to discover how Propio can simplify compliance and support your communication goals.